U.S. employees are seeking more intuitive, transparent and supportive pharmacy benefits, using tools that mirror the ease and simplicity of their favorite consumer apps, according to a new national survey commissioned by Evernorth and conducted by YouGov.
The study, based on responses from over 3,000 adults, highlights the growing expectations for digital convenience, cost transparency, and employer support in navigating prescription drug coverage.
Below we look at some key findings of the survey and offer considerations for employers to optimize coverage in their pharmacy benefit plans.
Good pharmacy benefits can drive productivity and loyalty
Employees who feel supported by their pharmacy benefits are more likely to be engaged and productive. In fact, 74% of working Americans with health benefits through their employer said they would work harder to help their workplace succeed if they are satisfied with the benefits their employer provides. However, only 38% said they trust their employer to act in their best interest when it comes to prescriptions, and just 37% agreed that their employer shows they care about them based on the pharmacy benefits they offer.
“These findings suggest that employees view pharmacy benefits as a valuable workplace perk, but many feel their employers are falling short in delivering a seamless and supportive experience,” said Ashley Holzworth-Nash, PharmD, vice president of retail network product strategy and solutions at Express Scripts. “A strong pharmacy benefit design coupled with effective communication can go a long way to improve employee satisfaction, enhance workforce loyalty and productivity.”

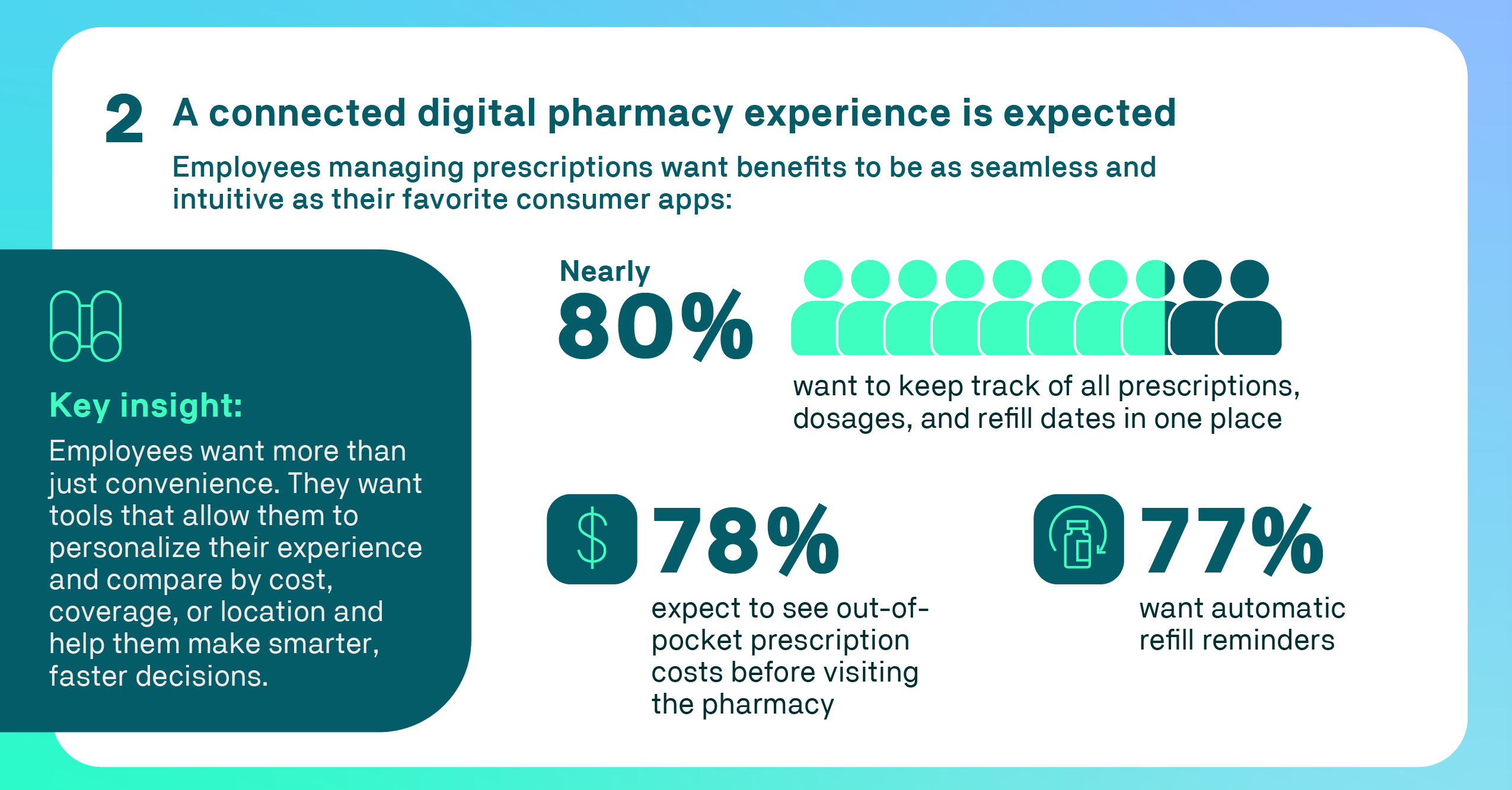
Employees expect app-like simplicity
The survey revealed a strong desire for pharmacy benefits that can be managed through modern consumer apps. Nearly 80% of employees managing their prescriptions want a centralized digital tool that can track prescriptions, dosages and refill dates. In addition, 78% want to see their exact out-of-pocket costs for prescriptions before they pick them up at the pharmacy, and 77% want to receive automatic refill reminders.
Respondents also expressed interest in features like real-time updates, seamless access across platforms, and tools to compare prices at nearby pharmacies – hallmarks of the consumer apps they use every day.
“These preferences reflect employees’ expectations for convenient digital-first experiences, with tools that connect them to helpful information personalized to their needs so they can make smarter, faster decisions,” Holzworth-Nash said.
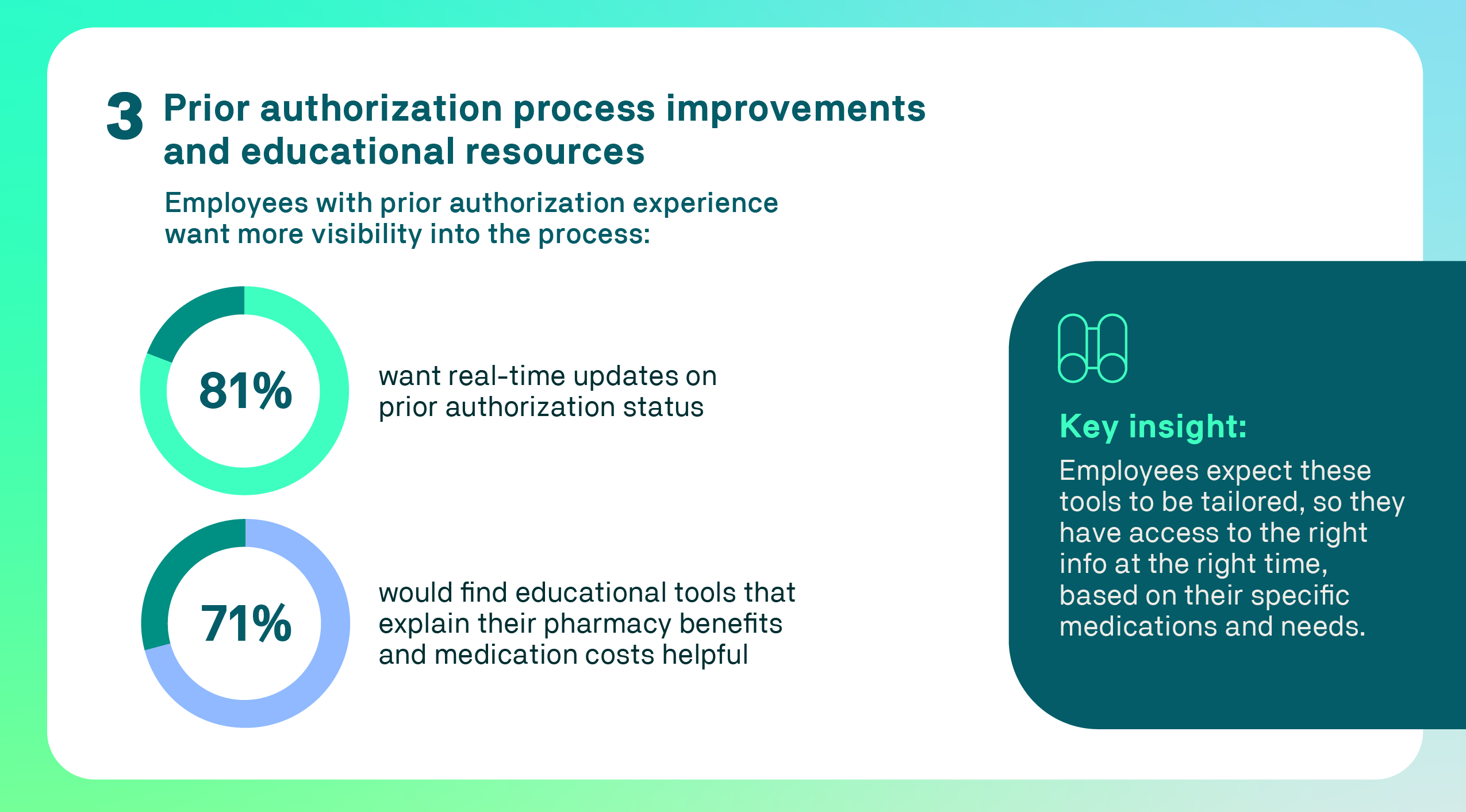
Visibility into prior authorization is a priority
Transparency in the prior authorization process was another top concern. Only 41% of employees who have experienced a prior authorization were informed about it by the prescribing health care provider when they wrote the prescription. Meanwhile, 29% learned about the need for prior authorization while the prescription was being processed, and 23% only found out when they tried to pick up their prescription at the pharmacy.
Among employees who experienced prior authorization for their prescriptions, 81% said they want real-time updates on the status of their requests. They also reported that online benefits portals (62%), text messages (55%) and pharmacy apps (53%) are the notification channels that help them feel the most informed about their prior authorization status.
Additionally, 71% of this employee group said they would find it helpful to receive clear explanations of how their pharmacy benefit works and how costs are calculated for their specific plan. Only 28% agreed their employer helps them navigate pharmacy benefits, and 44% disagreed outright, suggesting a gap in support that could affect employee trust and engagement at work.
“Educational tools that increase clarity of pharmacy benefit information – especially around prior authorization – can help reduce frustration and treatment delays, resulting in better outcomes and greater employee satisfaction,” Holzworth-Nash said.
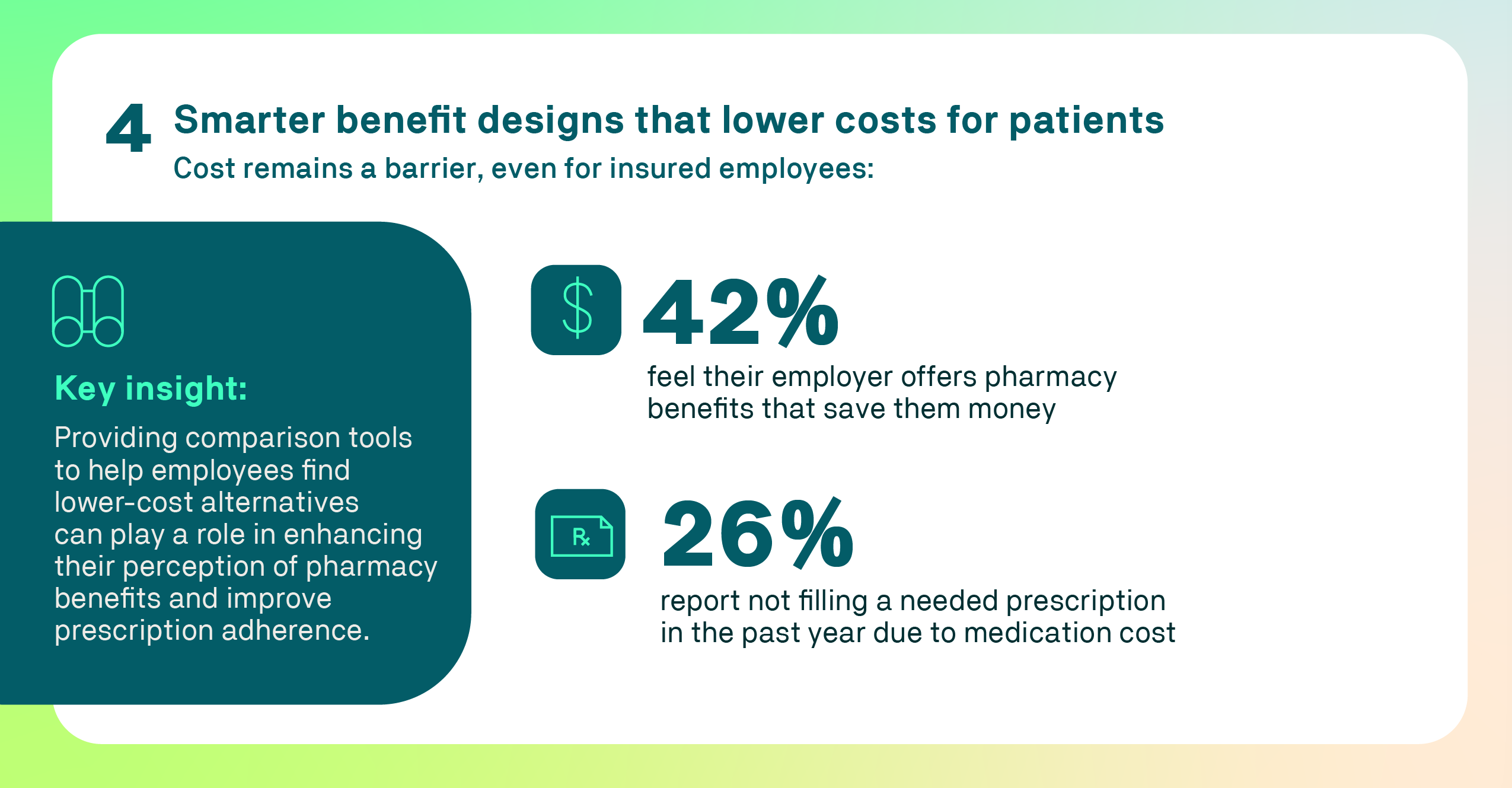
Cost concerns persist despite benefit coverage
Even with insurance, the cost of medication can still be a barrier for many employees. More than one quarter of employees (26%) reported not filling a needed prescription in the past year due to cost. Another 23% said they had paid more than expected for their medication, and 54% encountered an unexpected cost with their prescription.
Fortunately, 42% of employees feel their employer-provided pharmacy benefits help them save money, and roughly the same amount (45%) find their pharmacy benefits to be affordable. While many insured workers find value in their pharmacy coverage, a significant portion still struggles with affordability.
“It’s important for pharmacy benefit plans to be clear about expected out-of-pocket costs so there are no surprises,” Holzworth-Nash said. She added that offering comparison tools that help employees find more cost-effective options, such as generic alternatives, can help improve affordability and promote better prescription adherence, as well as boost satisfaction and trust in their employer’s benefit plan.
Delivering a simpler, smarter benefit experience
As employers look to strengthen workforce satisfaction and retention, pharmacy benefits represent a powerful opportunity to deliver meaningful employee support. Evernorth is committed to helping employers meet rising expectations by transforming the pharmacy benefit experience into one that is more intuitive, transparent and affordable.
“We’re focused on building a pharmacy experience that feels seamless and supportive – one that empowers employees to make confident, informed decisions about their care,” Holzworth-Nash said. “By simplifying access, improving visibility and delivering personalized guidance, we’re helping employers create benefit plans that truly work for their people.”


