Express Scripts, the pharmacy benefit services business at Evernorth Health Services, has always led the industry with innovation – guiding the pharmacy benefits landscape to meet the changing needs of plan sponsors, providers, patients, and the entire health care ecosystem.
Whatever issues evolve in the rapidly changing pharmacy landscape, Express Scripts is proactive in solving some of the biggest challenges in health care. “We move swiftly and strategically to ensure access to medications for patients who are simply trying to achieve better health,” said Adam Kautzner, president of Evernorth Care Management and Express Scripts.
Express Scripts began to challenge the industry status quo in 1989 by creating the first PBM drug formulary with the goal of guiding people to clinically sound, cost-effective medications. Express Scripts continued leading industry change, when it removed Lipitor, the top-selling brand-name drug at the time, from its formulary in favor of less expensive generics.
In subsequent years, Express Scripts launched an innovative program that delivered on the promise of hepatitis C cures without bankrupting health plans and then applied that program model to other costly drug classes, including PCSK9 cholesterol inhibitors and insulin to treat diabetes. Today, EncircleRx, which was introduced in 2024, is setting the standard for how to cover GLP-1s predictably and affordably, producing positive results for patients.
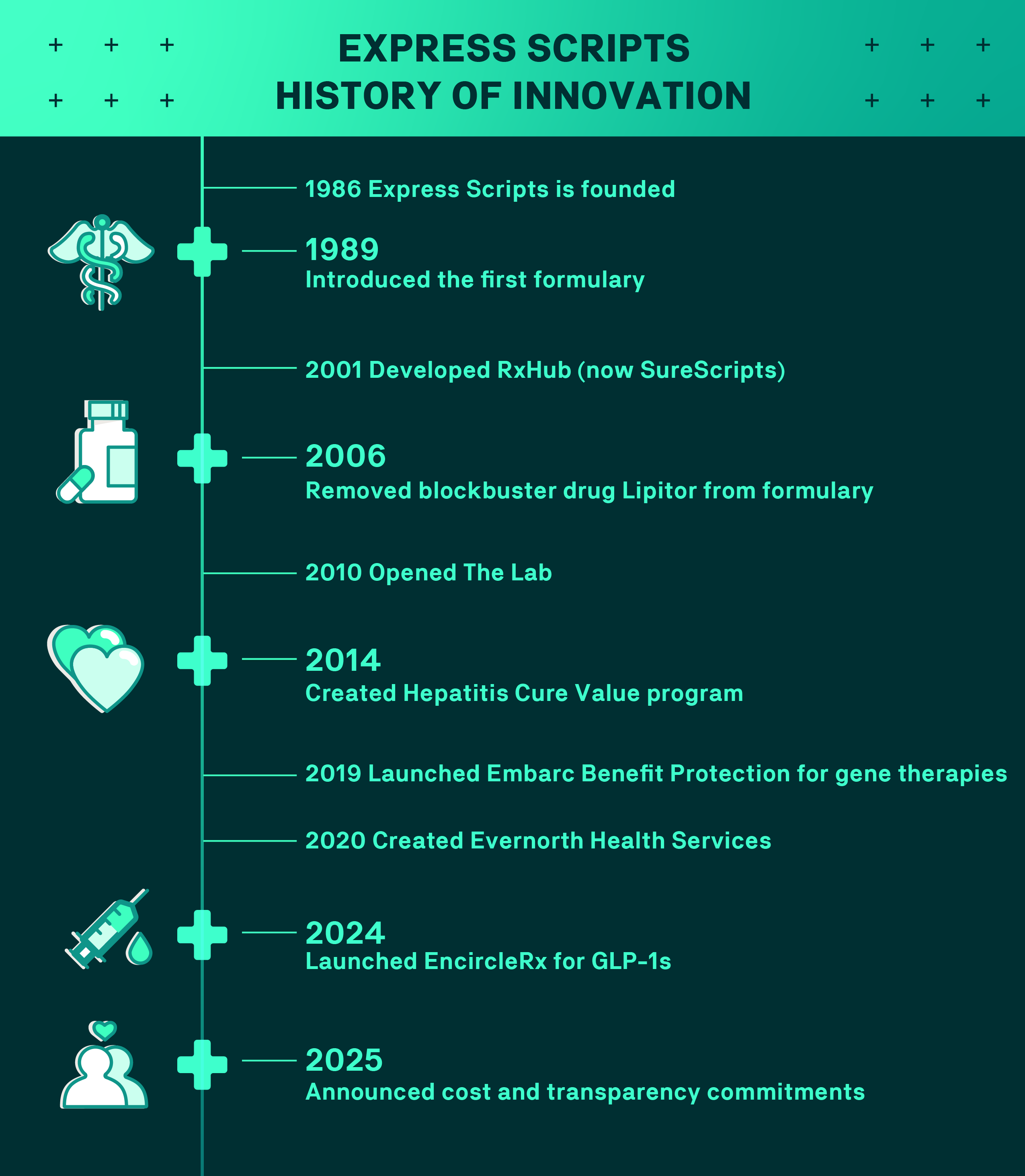
These are highlights in Express Scripts' innovation and not a complete list.
A commitment to transformation
Health care remains one of the most challenging industries to navigate, with numerous steps and decision points that can seem overwhelming for customers. Nearly 1 in 2 consumers report difficulties resolving insurance-related issues, and many are unable to reach a satisfactory resolution.
As the industry works to solve these issues, it must commit to address the pain points that keep people from getting the care they need.
For its part, Express Scripts recently announced it is working to help lower prescription drug costs by implementing protections to lower out-of-pocket costs for more patients. These actions are designed to help ensure patients receive the benefit of the savings Express Scripts generates through its negotiations. Express Scripts is also improving transparency through new standard reporting for patients and plan sponsors.
Express Scripts is working to improve its member experience in other ways as well. “We’re creating more connections and enhancing our standard member experience to provide more information, more choice, and more cost protections than ever before,” said Ashley Holzworth-Nash, Vice President of Product Management at Express Scripts. “We are making it easier for members to navigate their pharmacy benefits.”
Advocates for better health
Express Scripts is committed to making the health care system better and making people healthier by solving problems plaguing the system. The company is working to lead change so members understand how their pharmacy benefits are working for them.
“Many challenges are ahead of us – as are many opportunities,” Kautzner said. “Yet our vision for the future is clear: The needs of customers come first.”

