The COVID-19 pandemic accelerated the mental health crisis afflicting America’s youth. Diagnosed or undiagnosed, millions of young people are struggling, and many parents feel ill-equipped to manage the many related challenges impacting life at home and work.
The economic costs of the crisis are as staggering as the human costs. U.S. employers spend more than $200 billion annually on behavioral health costs for employees and their dependents, a figure that excludes indirect costs such as lost productivity and missed work.
“Despite growing attention, acceptance, and investments, the prevalence of mental health challenges continues to increase, along with associated direct and indirect costs,” said Eva Borden, president of Evernorth Behavioral Health. “We must change the trajectory of the crisis – and as powerful enablers of health and vitality through health insurance and benefits design, workplace culture, and community engagement, U.S. employers are uniquely positioned to address this pressing need.”
New research from the Evernorth Research Institute, along with survey data from YouGov commissioned by Evernorth, highlights the state of youth mental health and the depth of the challenges facing working parents who care for young people with mental health issues. The findings are a call to action for employers to strengthen their approach to behavioral health care to drive measurable, improved health outcomes.
Many young people are not receiving the full spectrum of behavioral health care
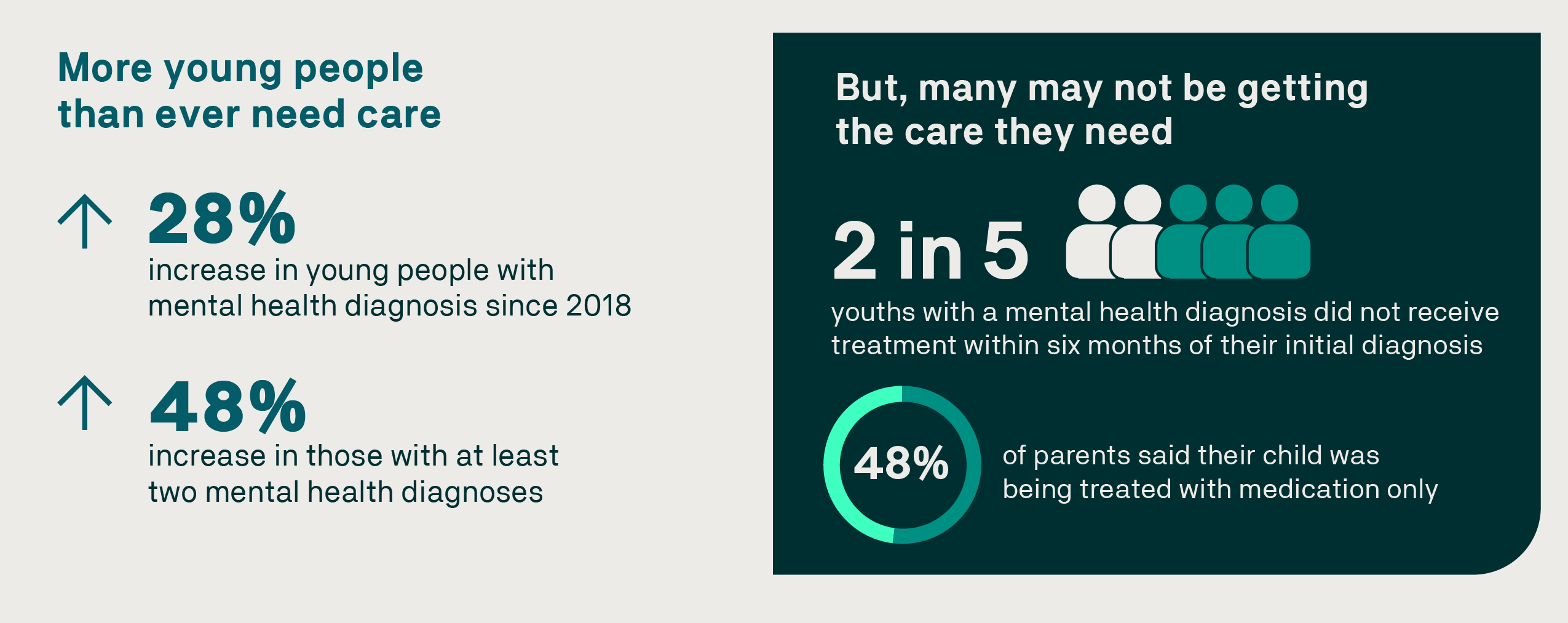
The youth mental health crisis persists. In our survey of U.S. adults, a quarter of parents said one or more of their children were experiencing mental health challenges, diagnosed or undiagnosed. The most prevalent conditions, based on our data, are acute stress disorders, ADHD, anxiety, and depression. While more young people are being diagnosed and more are receiving treatment, the data shows gaps, and many youths are not receiving the full spectrum of care.
Our research examined trends in youth mental health conditions based on claims data for more than 20 million commercially insured people under age 26. In 2022, 1.5 million of these young people had received a mental health diagnosis, a 28% increase since 2018. Thirty-eight percent (almost 2 in 5) did not receive treatment within six months of their initial diagnosis. Of those who did receive treatment, a significant number were treated with medication only.
Click here to view a larger version of this graphic.
According to the American Academy of Child and Adolescent Psychiatry, medication use in children should be considered as part of a holistic and collaborative mental health treatment plan. Not receiving the right care when needed often results in worse health outcomes and high cost escalations, and diminishes the ability of children and parents to engage at home, school or work, and in the community.
Every young person is different, and individual treatment plans determined by providers and parents are different. However, when youths are receiving medication only, adding therapy – individual or family – could provide an opportunity to improve and sustain health outcomes.
Working parents are struggling to tend to their child’s and their own mental health needs
More than half of parents reported challenges in trying to help their child feel better, with more than a one-third citing these barriers as the reason their child did not receive care.
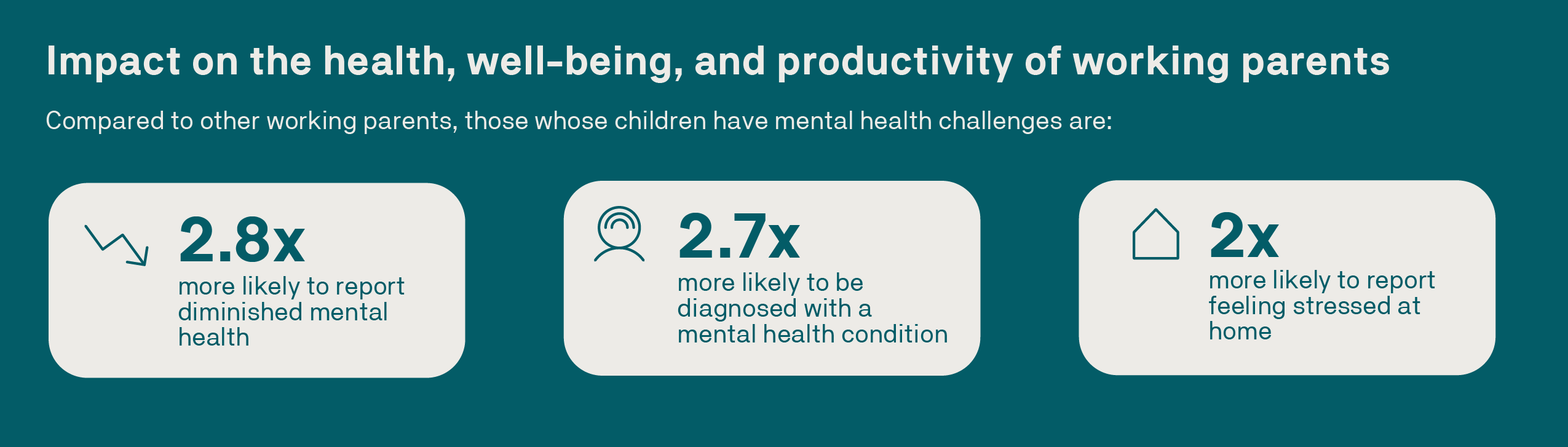
A majority (54%) of these parents reported a mental health diagnosis, making them 2.7 times more likely to be diagnosed with a mental health condition than working parents who do not have a child experiencing mental health challenges. They also report lower job satisfaction, find their jobs significantly more stressful, and are less able to carry out their job duties.
Click here to view a larger version of this graphic.
The more time a parent spends caring for a child’s mental health needs, the greater the disruption to their work. On average, working parents of a child with a mental health challenge spend about eight hours a week managing their child’s mental health needs.
Managing a child’s needs includes activities like looking for appointments, communicating with school staff, and learning about their child’s condition. On average, this disrupts up to four workdays a month, which can take the form of starting work late, leaving work early, or missing a full day of work.

Click here to view a larger version of this graphic.
Employers can do more to make it easier for parents to care for family mental health needs while meeting work responsibilities
Ensuring parents know how to recognize distress in children and when, where, and how to get the help they need builds confidence and increases the likelihood they will obtain help for their children and themselves. Employers can drive better behavioral health outcomes through the following:
Care delivery: Design a benefits approach that guides employees and families to evidence-based behavioral health treatment that integrates medical, behavioral, and pharmacy care, mitigating the potential for siloed treatment.
Customization: A data-driven, actionable approach to behavioral health care allows for personalized plans to assess, treat, and offer better care at every touchpoint.
Culture: Cultivate an environment that helps alleviate stigma, educates employees and managers, and acknowledges and addresses social determinants of health (SDOH).
Community engagement: Employers can support individual, workplace, and community connectivity to address some of the underlying drivers of mental health challenges.

Click here to view a larger version of this graphic.
“A stronger, more effective approach to behavioral health care focuses on quality, evidence-based care, addresses access gaps, and simplifies care navigation to drive better health outcomes for children and parents – along with enabling a healthier, stronger U.S. workforce,” Borden said. “Areas of opportunity to drive better behavioral health outcomes include care delivery, custom data-driven approaches, workplace culture, and community engagement.”
Evernorth is committed to improving youth mental health
We’ve made important progress expanding access to evidence-based, quality, in-network therapy for millions of people through the Evernorth Behavioral Care Group. We’re launching an innovative measurement-based care program for our behavioral health network, expanding and promoting utilization of virtual care, and advocating for provider self-identification in specialty areas, including those working with children and teens.
This article was created with the assistance of AI tools. It was reviewed, edited, and fact-checked by Evernorth’s editorial team and subject matter experts.


