Pharmaceutical innovations – and costs – are an important part of any discussion about where our health care system is today and where it is headed. Over the last 12 months, Express Scripts, the pharmacy benefits management (PBM) business of Evernorth, has rolled out numerous groundbreaking programs and offerings to help Express Scripts’ 100 million members get the medicines they need, when they need them, while driving greater medication affordability for patients and plan sponsors.
Read on to learn about some of the most notable advancements and innovations of 2023.
Partnering with independent pharmacies to expand access to health care
In rural locations and other areas across the United States, the demand for health care services far outstrips the supply of pharmacies, hospitals, clinics, and medical providers. Getting timely care can be difficult, and those who are unable to drive long distances may find it close to impossible. At the same time, a growing shortage of doctors threatens to worsen the situation.
In the spring of 2023, Express Scripts launched its IndependentRx Initiative to enable independent pharmacists to close some of these gaps in care while offering increased reimbursement opportunities. In addition to dispensing medications and administering vaccines, pharmacists have the expertise and training to be a resource for direct patient care, said Stephanie Smith Cooney, senior director of independent pharmacy affairs.
“We’re committed to leveraging and supporting the clinical expertise of pharmacists who want to do more for their patients,” said Adam Kautzner, president of Express Scripts. “By deepening our partnership, together we will remove barriers to care, reduce total medical costs, and improve vitality, community by community across the U.S.”
Cooney, who joined Express Scripts in the summer of 2023, also leads the Independent Pharmacy Advisory Committee, which is charged with expanding the role of rural, suburban, and urban pharmacies in the health care system. The committee, a group of 39 pharmacists representing every region in the U.S., held its inaugural meeting in November.
“Our first meeting set the stage for this important work,” Cooney said. “Our goal is to ensure access to health care for all who need it by leveraging the value that independent pharmacies bring to the health care system.”
Simplifying drug costs for members and clients
This year, Express Scripts launched the Copay Assurance plan. Even if they have not met their deductible levels, members whose health plans opt into the plan will pay no more than $5 for each fill of generic and specialty generic prescriptions, $25 for preferred brand drugs, and $45 for preferred specialty brand drugs. The Copay Assurance plan is in addition to the Patient Assurance Program, which since 2020 has capped out-of-pocket costs for insulin and other diabetes treatments at $25 for up to a 34-day supply (or $75 for a 90-day supply) for the more than 11 million members enrolled in the program.
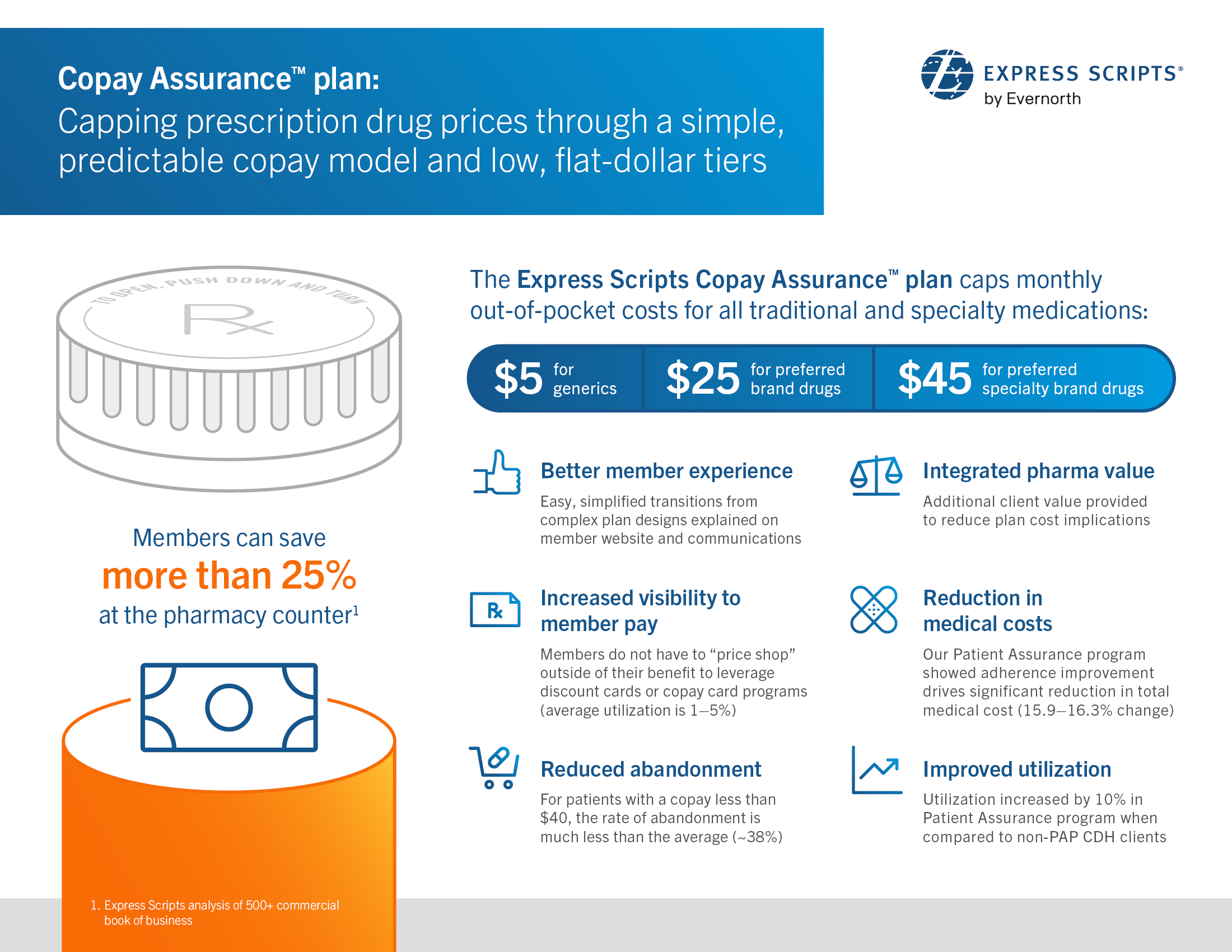
Click here to view a larger version. Express Scripts’ new Copay Assurance™ plan ensures consumers pay less out-of-pocket by capping copays on prescription drugs at $5 for generics, $25 for preferred brand drugs, and $45 for preferred specialty brand drugs.
In November, Express Scripts added a new pharmacy network option, Express Scripts ClearNetwork, which standardizes and simplifies payments to pharmacies. Many clients – including most employers, government organizations, and health plans – can opt into the network, which will offer pricing based on industry benchmarks for prescription drugs and pharmacy services and a seamless experience for customers filling prescriptions. The network, which will become available early in 2024, will apply to all prescription drugs on a plan sponsor’s list of covered generic, branded, and specialty medications.
“This new model differs from other pricing options where Express Scripts negotiates discounts with pharmacies to meet guaranteed rates for clients,” Kautzner said. “Express Scripts ClearNetwork is a simple pricing option that reinforces the value of our work to help consumers easily access the medications they need, while also shining a light on the root cause of high drug costs – drug manufacturers who set and raise prices.”
Expanding access to biological medications by encouraging competition
Biologic therapies derived from living organisms such as blood, cells, tissues or proteins have been around for more than a century and include treatments such as insulin. In recent years, highly sophisticated versions have been developed, often offering hope to patients with chronic inflammatory conditions such as rheumatoid arthritis and Crohn’s disease. One such biologic, Humira, is the top selling pharmaceutical drug in the world – and as its market share increased, its list price soared 470%.
The introduction of biosimilars is changing that dynamic. These lower cost, clinically equivalent alternatives are creating competition in the market, which can ultimately lower costs for patients and their health plans. Biosimilars determined by the FDA to be interchangeable can be dispensed when their originator biologic is prescribed, much like generics can be dispensed in place of brand drugs. In 2023, Express Scripts added three biosimilars to Humira to its largest formulary.
Evernorth analysis estimates that competition created with biosimilars can save the U.S. $225 billion to $375 billion in total pharmacy spend over the next decade. These potential cost savings are in evidence when tracking the list price of the long-acting insulin injector Lantus, which more than doubled during the five years after it gained FDA approval in 2010. The price fell when competing products entered the market in 2015 and continued to decrease following the entry of several biosimilar options — including an interchangeable option in 2021.
"Embracing biosimilars as they come to market builds on our efforts over the past decade to support greater adoption, just as we did when generics first became available over 30 years ago,” Kautzner said.



