There’s no easy answer to the challenges faced due to the COVID-19 pandemic. And, although COVID-19 is not officially an endemic, most agree it’s here to stay.
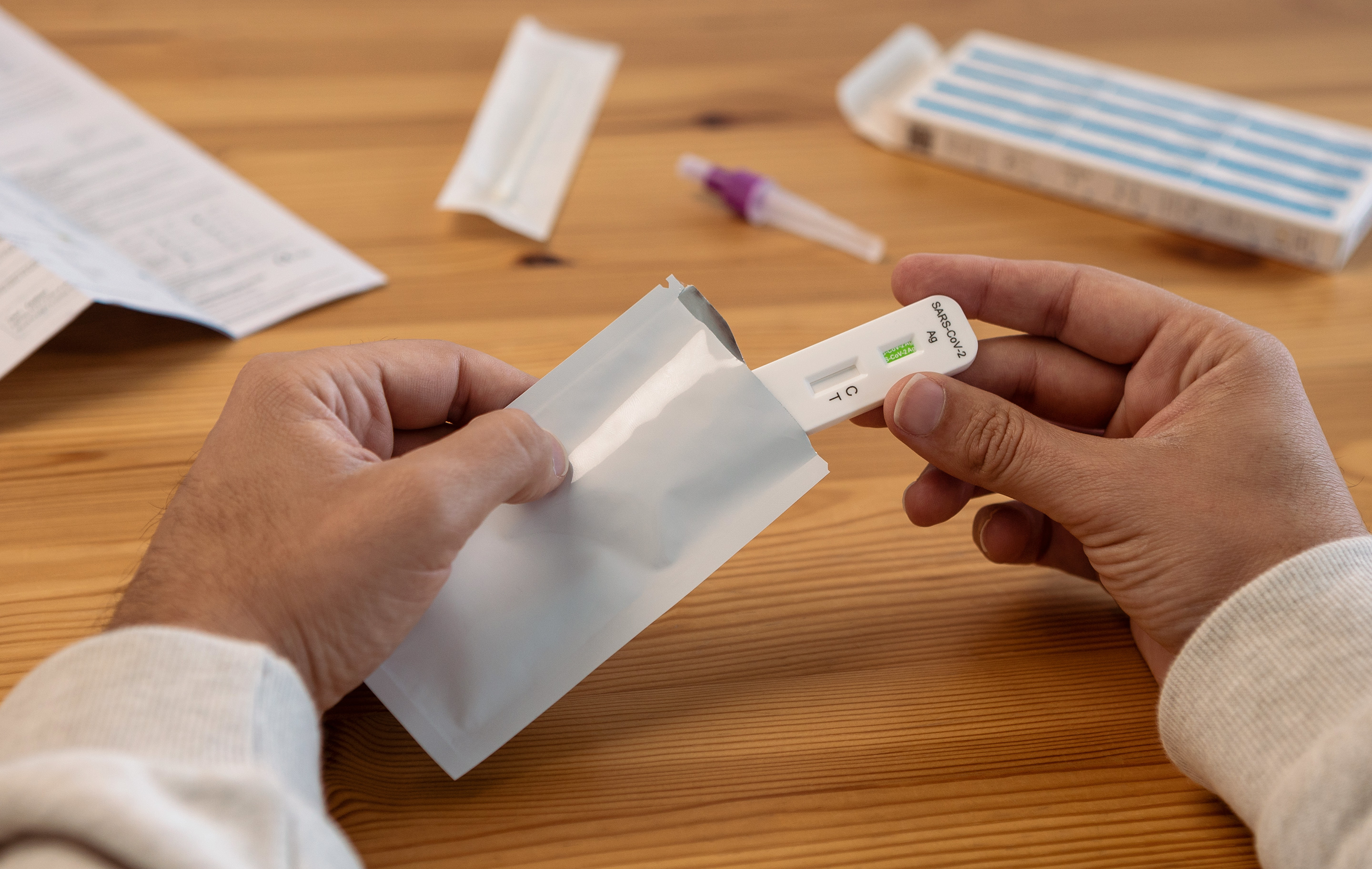
Over-the-counter home test kits
Starting May 12, 2023, plan sponsors are no longer required to pay for COVID-19 over-the-counter (OTC) tests. But, just because it’s not required doesn’t mean it’s not a valuable benefit to offer. A positive test helps your members get treated faster and take steps to minimize the spread of the virus. OTC tests can also be used to show negative results if required for work, school, travel, visiting family in a nursing home, and many other reasons. It’s recommended for plan sponsors to continue covering the cost of at least 4 test kits per member per month at $0 member copay. On top of offering test kits at local retail pharmacies, if allowed by state law, plan sponsors should also offer a home delivery option.
Vaccination and booster shot coverage
Under Section 2713 of the Affordable Care Act (ACA), non-grandfathered private insurers and self-insured employer plans must provide coverage for a range of recommended preventive services and may not impose cost-sharing (such as copayments, deductibles, or co-insurance) on patients receiving these services.
The preventive services guidelines require coverage for adults and children and include COVID-19 vaccinations and boosters recommended and determined to be for routine use by the Advisory Committee on Immunization Practices (ACIP).
COVID-19 oral antiviral therapeutics program
Antivirals will see no changes post-PHE. The U.S. Food and Drug Administration (FDA) has not yet approved these drugs. The only product currently available is under an emergency use authorization (EUA).
Pharmacists have been granted new prescribing authority from the FDA, allowing them to prescribe PAXLOVIDTM to eligible patients testing positive for COVID-19. When Paxlovid is prescribed and dispensed by a pharmacist, the savings are substantial, for both plans and patients. The best ways for plans to take advantage of this to maximize savings and health outcomes are:
- Ensuring members have access to participating pharmacies nationwide
- Setting up the benefit with $0 member copay
- Communicating to members about what antivirals would be available to them and how to get a prescription from a pharmacist instead of the doctor’s office or emergency room.
We project that plan sponsors can expect up to a 50% decrease in plan spend when members see a pharmacist vs. a physician for a Paxlovid prescription.1
While COVID-19 is no longer classified as a public health emergency, it’s here to stay, which means that it’s important for plan sponsors to continue providing COVID-19-related coverage and care to keep members healthy and plan costs low.