The confluence of escalating costs, rapid technological advancements, and ongoing lifestyle and health services utilization issues have created unprecedented challenges for the U.S. health care system, according to research released this month in the new edition of the Health Care in Focus report.
The Evernorth Research Institute partnered with Ipsos to conduct a nationwide survey of benefit decision makers, health plan leaders, and consumers. Our analysis revealed insights that highlight the importance of human-centered care that balances technological advancements and other innovations with personalized engagement.
Read on to learn more about some of the challenges we uncovered, plus actionable insights for plan sponsors that can help make health care more efficient, sustainable, and accessible for all.
Managing escalating costs
Health care spending in the U.S. reached $4.5 trillion in 2022, an average of about $13,500 per person and a 4.1% increase from the previous year. This amount is more than double the per capita spend of other high-income countries. Among U.S. adults covered by health plans, a large majority cited concerns about being able to afford medical costs, including 80% of Hispanic-identifying consumers and 74% of white consumers. Additionally, 73% of millennials and 68% of baby boomers are concerned about losing access to their current health care plan.
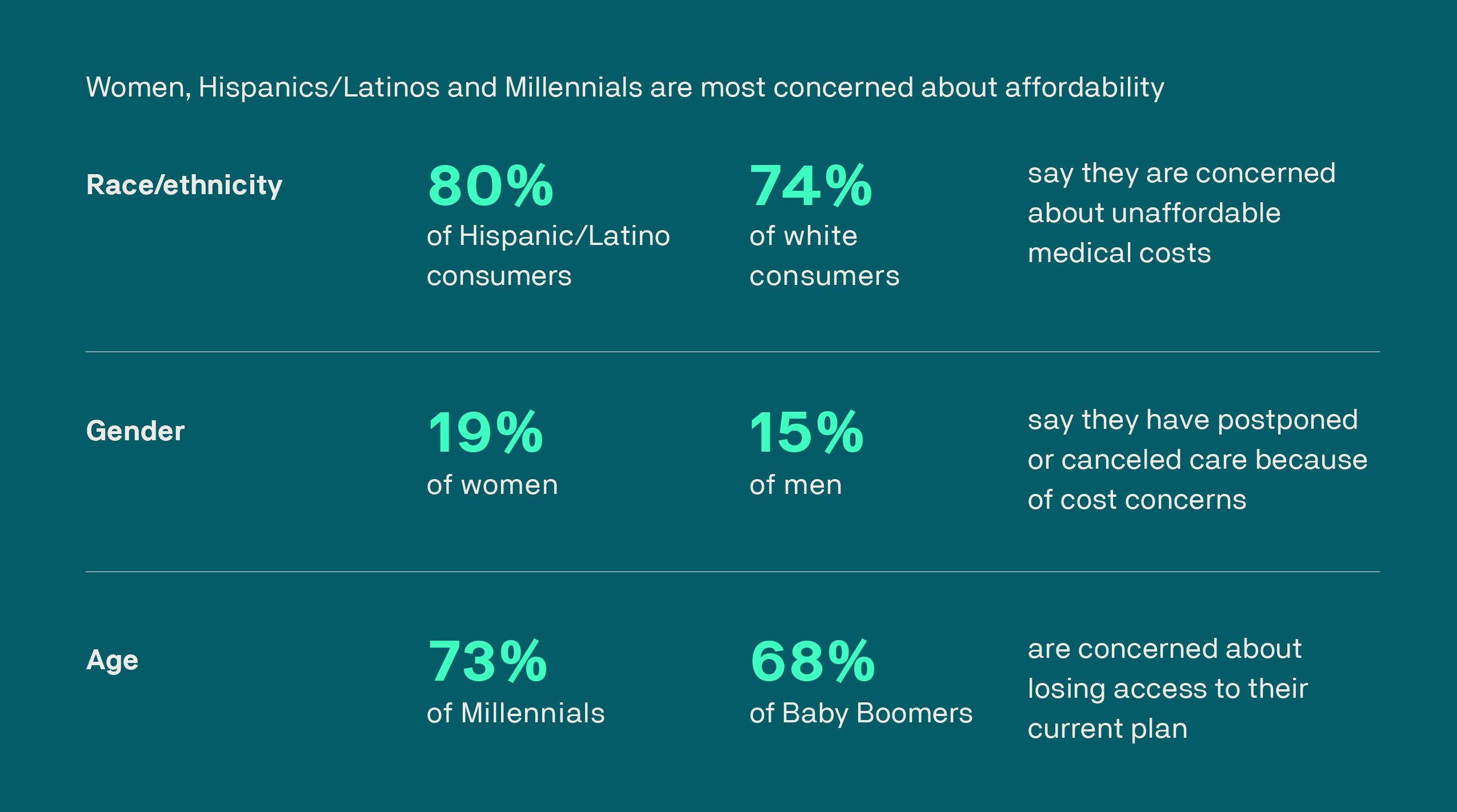
Click here to view a larger version of this graphic.
Financial concerns are especially prevalent in underserved communities, where people worry about paying for housing, food, education, health care, and other essential needs.
Insight:
By increasing investment in whole-person health strategies that focus on wellness and extend beyond traditional care, plan sponsors can improve their members’ ability to stay healthy and obtain the health services they need while minimizing financial hardship.
Determining how to use artificial intelligence (AI)
AI is among the many technological innovations finding a place in health care, yet only 61% of consumers say they are comfortable with the use of AI in health care, compared with 93% of employers and 96% of health plan leaders. Nine out of 10 consumers agreed that in-person interaction with their providers is vital to managing their health.
When asked about specific uses of AI, however, 71% of consumers said AI should be used to identify possible interactions between medications, 68% said the technology should be used to facilitate their providers’ administrative tasks, and 67% said AI should be utilized to clarify their health benefits.
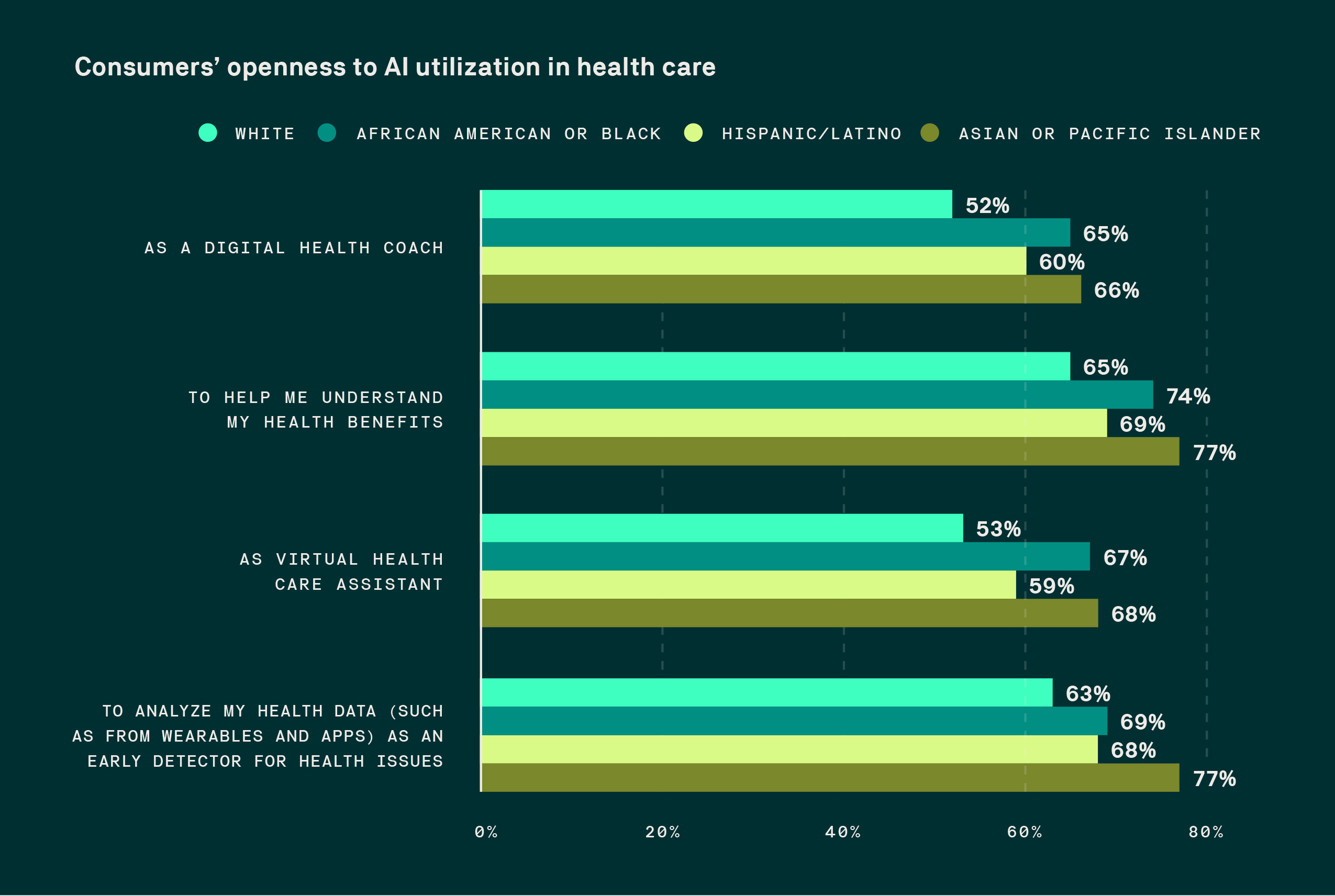
Click here to view a larger version of this graphic.
Insight:
When health plans and providers adopt AI tools that leverage data to support patients and clinicians in making informed decisions, we can more fully realize the benefits of the technological advancements in health care. Coupling AI with compassionate health care practices and personalized education can help lead to better patient outcomes and experiences.
Improving health literacy
Our research shows that lack of awareness, option overload, and the complexity of today’s care delivery systems keep people from utilizing the right care at the right time. While rapidly accelerating advancements in technology promise improved outcomes, they also lead to an overwhelming amount of information for consumers. This can trigger decision paralysis, when people struggle to make informed health care decisions due to the volume and complexity of their options.
About two-thirds of U.S. adults say managing care is overwhelming and time consuming, and a similar number have trouble understanding which benefits or solutions to use. For example, many consumers are unaware that they have access to employee assistance plans (EAPs), which provide one-on-one help to connect them with behavioral health providers, often at no cost for their initial visits.
In contrast, adults who have a clear understanding of their health conditions and the health care system are more likely to engage in preventive care, adhere to prescribed treatments, and make informed decisions regarding their health. As a result, they are more likely to use health care services appropriately, reducing unnecessary and costly emergency department visits and hospitalizations.
Insight:
By focusing on personalized learning and customized communications to increase health and health insurance literacy, plan sponsors can offer clear, concise guidance that helps members navigate and use their benefit options effectively.
This article was created with the assistance of AI tools. It was reviewed, edited, and fact-checked by Evernorth’s editorial team and subject matter experts.



