Access to prescription medications and affordability remain significant challenges for many Americans. According to recent studies, a substantial number of individuals in the United States report rationing doses or not filling prescriptions due to cost concerns, which can lead to worsening health and increased medical expenses in the long run.
To lower the cost of medication for the Americans we serve, Evernorth Health Services announced a new pharmacy benefit model for Express Scripts that will deliver immediate savings and greater transparency to patients when they are picking up their medications at the pharmacy counter – marking a significant departure from the traditional rebate system.
“The pharmacy benefit model has delivered significant value over the years, helping manage drug costs and improve access, especially when it comes to generics and biosimilars,” said Ashley Holzworth-Nash, vice president of product management at Evernorth. “However, today more than ever we know that Americans expect transparency and greater affordability in health care. We are responding to that market demand, while launching what we believe to be the next era of pharmacy benefits.”
A rebate-free model for greater affordability and transparency
In the traditional pharmacy benefits model, pharmacy benefit managers (PBMs) like Express Scripts negotiate rebates with drug manufacturers. These rebates are paid after the medication is purchased. Critics say this makes it more difficult for patients to understand where the savings go and how they impact out-of-pocket costs.
The new Express Scripts model changes that by applying discounts at the point of sale, allowing patients to pay less for their medications on the spot. “This is a major step forward for patients,” Holzworth-Nash said. “Patients benefit from lower brand drug prices at the pharmacy counter. This makes the experience simple and predictable.”
The new model will be implemented for members of Cigna Healthcare’s fully insured plans in 2027. The model will become the standard option for all Evernorth pharmacy benefits clients in 2028.
Holzworth-Nash noted that the new model will be especially helpful for people enrolled in high-deductible health plans or those who pay the full cost of their prescriptions. For them, the cost of brand-name drugs could drop by an average of 30%. Lower upfront costs lead to better medication adherence, improved health outcomes, and greater trust in the health care system.
Ensuring the lowest available price
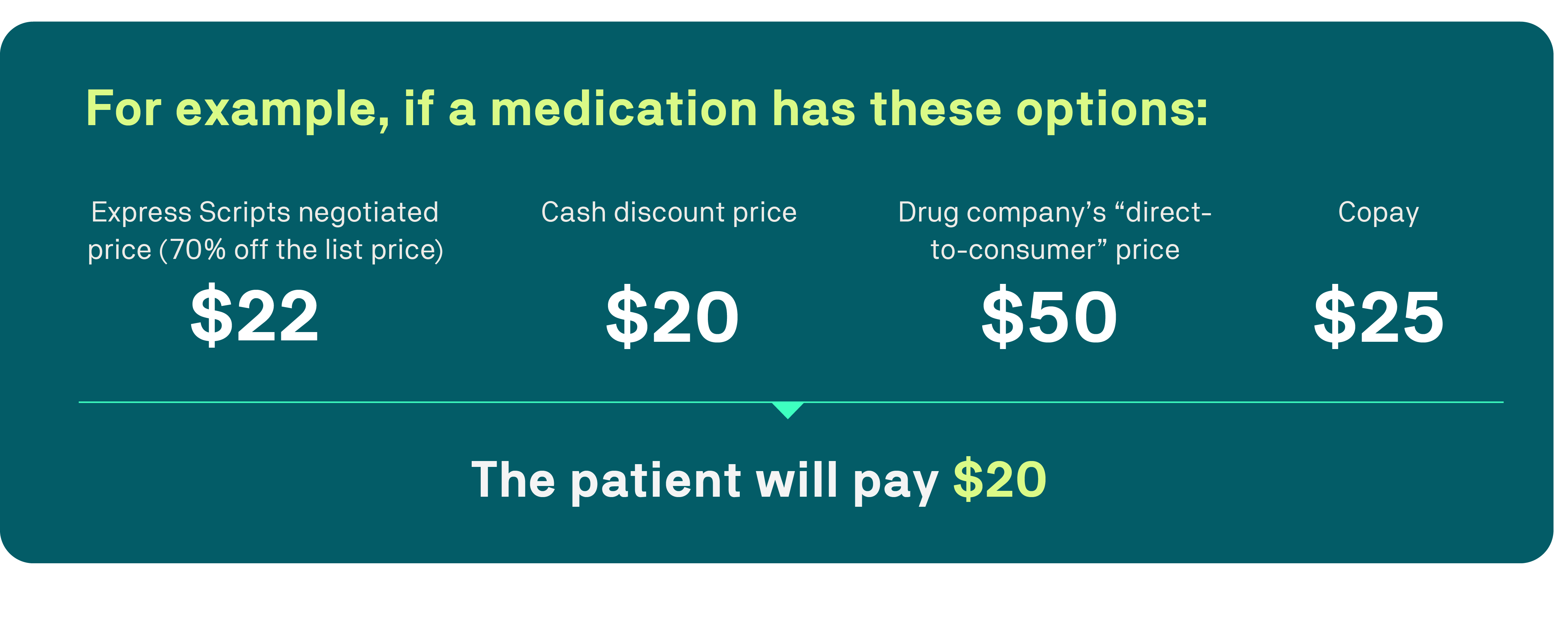
Evernorth also leverages technology to ensure patients pay the lowest pricing option for both brand-name and generic medicines – whether it is the Express Scripts negotiated price, their copay, a cash discount, or the drug manufacturer’s direct-to-consumer price. Currently, tens of millions of patients already benefit from this technology and millions more will start benefiting starting January 2026. Evernorth plans to incorporate this model with upcoming direct-to-consumer programs as they become available to ensure patients have the lowest cost option available.
Protecting access to community pharmacies
Evernorth recognizes the critical role community pharmacies play in providing care to patients in their area, including some of the most vulnerable populations across the country. The new Express Scripts model will leverage a reimbursement structure that compensates pharmacies based on their cost for medications plus a dispensing fee.
Additionally, the new model will introduce performance-based reimbursement that rewards pharmacies for quality patient care, rather than being compensated solely for dispensing medications. This model will further expand the focus on opening the doors of community pharmacies to play a larger part in delivering care to the Americans they serve. This means pharmacies are compensated for the clinical services they provide and outcomes that plan sponsors select, such as medication adherence, generic dispensing rates, medication counseling, and immunization rates – which means enhanced quality of care for patients.
“With this pharmacy reimbursement model, we expect that patients will experience better medication adherence, improved health outcomes, lower costs, and more integrated, transparent care,” Holzworth-Nash said.
Overall, the new Express Scripts model is the next step toward a simpler and more supportive pharmacy care experience. With lower costs at the counter, clearer price information, and pharmacies focused on outcomes, patients will be in a better position to manage their medications and stay on track with their health.


