Prescription drug rebates happen behind the scenes, but they provide significant benefits, lowering costs for plan sponsors – which enables lower premiums or other cost-sharing methods for their members.
Demystifying drug manufacturer rebates
Drug manufacturers set list prices for brand-name drugs, and these list prices generally increase year over year. That’s where pharmacy benefit managers (PBMs) like Express Scripts play a valuable role. PBMs reduce the net cost of drugs in the most expensive therapy classes so plan sponsors and their members don’t bear the full brunt of high drug prices.
Lowering drug costs through PBM negotiations
PBMs negotiate with pharmaceutical companies on behalf of their clients and members to lower the cost of medications included on clients' formularies. Formularies, also known as drug lists, contain clinically sound and cost-effective medications that plan sponsors offer as part of their pharmacy benefits.
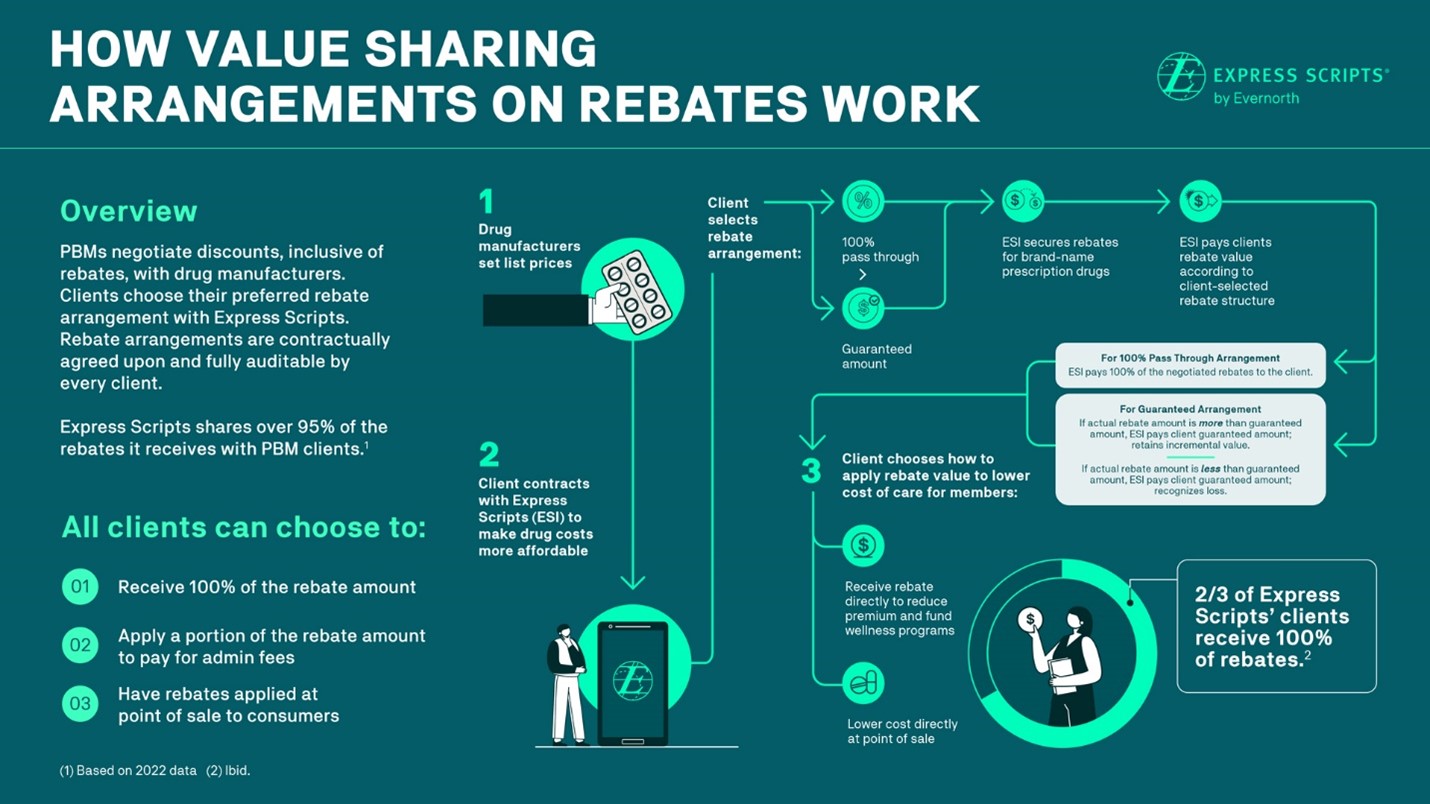
As part of the negotiation process, drug manufacturers offer rebates on many – but not all – brand-name medications. When a patient fills a prescription for a medication that carries a rebate, the manufacturer remits the appropriate amount to the PBM, and the PBM shares that value with the patient’s plan sponsor according to the terms of their contract. Express Scripts’ clients receive 95% of the drug rebates that we obtain by negotiating with pharmaceutical companies. Express Scripts gets paid to cover the administration of the client’s pharmacy benefit, including services such as reporting and analytics. The client always has the right to audit based on their contract.
Drug rebates and transparency
Drug rebates are sometimes mischaracterized as secret or hidden payments. The opposite is true: Clients have insight into the rebates Express Scripts secures, and they can use rebate value to help manage the cost of their overall benefits budget. They choose from multiple economic models that provide clear and predictable costs for prescription drug benefits. These financial arrangements include the option of an annual audit, at no cost to clients.
In addition, Express Scripts’ clients have full transparency and choice in how they choose to direct their rebate dollars and how to utilize their savings. They can use the rebate value in a variety of ways, including lowering the total cost of care through lower premiums and cost sharing, offering expanded medication lists, providing funding for wellness programs, and reducing the amount their members pay for the medicine at the pharmacy counter.
Click here to view a larger version of this image in a new window.
PBMs: Driving affordability in innovative ways
Rebates are just one of the tools PBMs use to help our clients ensure consumers can access affordable medications. Especially today, PBMs play a key role in driving greater competition and lowering costs.
For example, list prices for commonly used brand-name medications rose 36% from 2016 to 2021, while the prices for common household goods increased 10% in the same period. Today, the average American spends more than $1,100 a year on prescription drugs.
While rebates are one way to drive competition and lower costs, PBMs have developed numerous innovative tools to optimize affordability for plan sponsors and patients, such as managing specialty drug costs while preserving access to life-sustaining and life-saving therapies. PBMs are projected to deliver a total of $1 trillion in savings on drug costs over the next decade.
Working with the complex drug supply chain in the United States, PBMs will continue to drive competition to lower costs and combat the already high – and rising – price of prescription medications. In doing so, we are saving money for employers, health plans, government entities, and the health systems that hire us.



